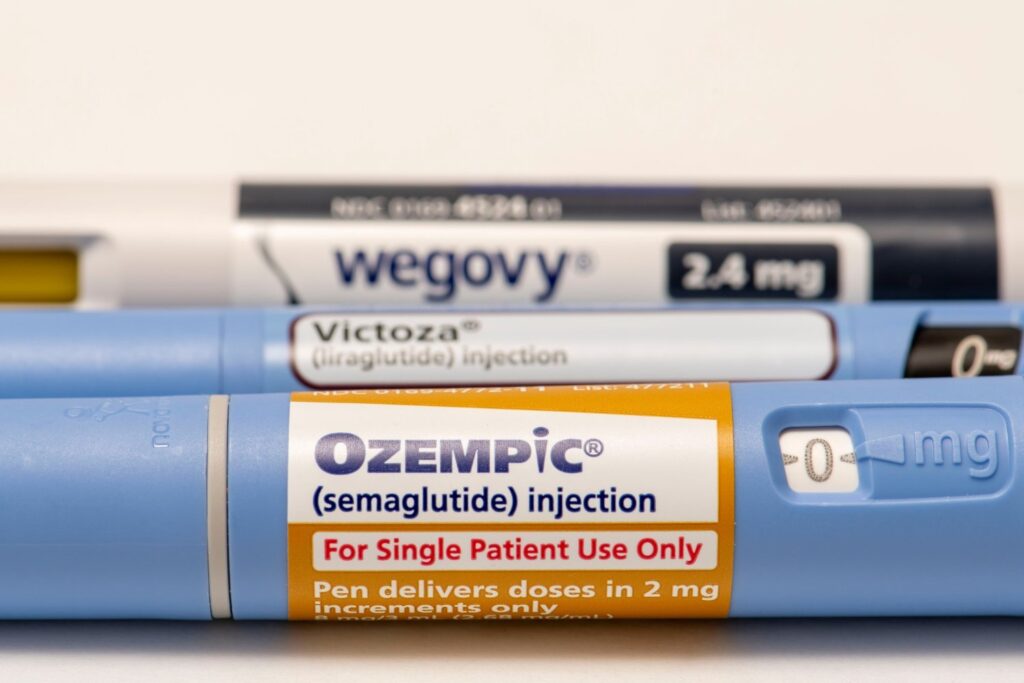
Ozempic, Wegovy and their ilk have become the pharmaceutical darlings of the 2020s. These drugs can help people lose more weight than diet and exercise alone, and research is starting to find that their benefits may extend further. But what exactly makes them work, and why do they seem to affect so many different aspects of our health?
The link between poor health and weight gain is always more complex than is often portrayed. But obese people do face a greater risk of some health problems, and many people do want to lose weight for understandable reasons, such as being able to relieve knee pain or sleep more soundly without apnea. Unfortunately, as most people who have tried to lose weight will tell you, it’s very difficult to lose significant amounts of weight and keep it off long-term.
The advent of Ozempic and its ilk has dramatically changed this reality, but despite their effectiveness, there are still many misconceptions and mysteries surrounding how these drugs work.
powerful imitator
The active ingredient in Novo Nordisk’s Ozempic and Wegovy is semaglutide, which officially belongs to a group of drugs called glucagon-like peptide 1 receptor agonists, or GLP-1RA. GLP-1 is one of several hormones that play key roles in regulating metabolism and hunger. It does this through a variety of mechanisms.
For example, when we eat, our blood sugar starts to rise. In response, the gut releases GLP-1, which stimulates the pancreas to produce insulin, which then moves glucose from the blood into cells, lowering blood sugar levels. GLP-1 also interacts with the vagus nerve to slow the emptying of food in the stomach, helping to create a feeling of fullness when we eat. Certain cells in the brain also produce GLP-1, and this brain GLP-1 is thought to suppress our appetite and food cravings throughout the day.
Scientists first discovered GLP-1 in 1986 and soon discovered its direct effect on insulin, leading scientists to wonder whether GLP-1 or something very similar could be used to treat type 2 diabetes – a disease characterized by uncontrolled and chronic diseases. However, natural GLP-1 does not last long in our bodies, with a half-life of only a few minutes. Eventually, scientists were able to develop a lab-made protein that activates the same receptor as GLP-1 while lasting longer in our systems, called GLP-1RA.
The first GLP-1RA drug approved for type 2 diabetes was exenatide, a synthetic version of a protein (extenin-4) that was first discovered in the saliva venom of the Gila monster.Suspected viper venom). Other GLP-1RAs have been launched over the years, with semaglutide first approved in 2017 as the diabetes drug Ozempic. Endocrinologist and Medical Director of the Medical Weight Program at Carolina University.
“When they start producing these synthetic versions and making some modifications to them, they actually just extend the half-life,” Covello told Gizmodo over the phone. In particular, semaglutide has a half-life of approximately one week, which is much higher than exenatide’s approximately 13 hours. One major modification of semaglutide prevents it from being broken down quickly by the DPP-4 enzyme, while another modification allows it to bind tightly to the serum protein albumin, meaning it can stay in our bloodstream longer. , without being filtered out by the kidneys.
Although GLP-1RAs were originally developed as a treatment for type 2 diabetes, scientists as early as the 1990s suspected that they could also be used to treat obesity, given GLP-1’s effects on hunger and satiety. The first GLP-1RA approved for obesity was liraglutide, marketed as Saxenda, approved in 2014, while a higher-dose version of semaglutide was approved in 2021, marketed as Wegovy.
What are the advantages of GLP-1?
As valuable as these early GLP-1 drugs were to patients, the arrival of semaglutide truly changed the paradigm of obesity medicine. In large-scale clinical trials, people taking Wegovy lost about 15 percent of their weight over a year, far greater than the typical success of diet and exercise alone and greater than the typical success of older weight-loss drugs. By comparison, people taking Saxenda in a similar trial lost about 7.5% of their body weight.
Some studies suggest that obese people produce less natural GLP-1 in response to food, which may help explain their higher weight. Given this, it is tempting to think that these drugs simply repair GLP-1 deficiencies in obese people. However, this study is not conclusive and obesity is often a complex disease with many different interacting factors. It may be more accurate to say that GLP-1RA is a particularly potent lever, if not the only one available, that we can use to address the biological basis of obesity. That said, people taking these medications often experience a significant sense of relief, often reporting a significant reduction in “food noises” or persistent intrusive thoughts about food.
In the years since Wegovy’s approval, GLP-1RA’s benefits not only for obesity but also for many other health conditions have been solidified. Large studies have found that semaglutide can reduce the risk of heart and kidney problems in obese people at high risk; others have found early evidence that GLP-1RA can reduce the risk of obesity-related cancers, depression and even dementia. Most of these benefits appear to be related to the substantial weight loss induced by GLP-1 therapy. While obese people are not necessarily less healthy than the average person, obesity is associated with higher levels of inflammation, high blood pressure, and other body changes that may increase our risk of health problems such as type 2 diabetes and heart disease. Therefore, weight loss may better improve these factors, but this alone does not explain all of the optimistic benefits that may be associated with these drugs.
Some studies suggest that semaglutide may improve heart health even in people who have lost little weight, possibly because of its blood sugar-lowering or inflammatory effects. Other studies have found preliminary data showing that semaglutide can curb cravings for unhealthy habits like alcohol and gambling—an unexpected phenomenon that may be related to GLP-1’s role in the brain.
It turns out that the role of natural GLP-1 in regulating food intake appears to come primarily from GLP-1 in the brain rather than in the gut. GLP-1 receptors in the brain also appear to play a role in regulating our responses to potentially addictive stimuli such as cocaine and other drugs, possibly through interactions with dopamine, a neurotransmitter closely linked to our reward system matter) interact, although scientists are still unsure about the exact mechanisms involved. Regardless, researchers have begun larger trials of semaglutide as a treatment not only for alcoholism but also for other brain-related conditions such as Alzheimer’s disease.
What’s wrong with GLP-1?
No drug is risk-free, and GLP-1RA is no exception. Their most common side effects are gastrointestinal symptoms such as nausea, vomiting, and constipation. Coviello said these could also be explained by the biological properties of GLP-1.
“So when these compounds are present for a few hours, you may get some potentially beneficial effects, such as slowing down intestinal motility, which allows you to digest food more efficiently,” she explains. “But if you extend the half-life to one day, or now seven days a week, we think that the slowing of intestinal motility is what’s behind this feeling of fullness and maybe some of the nausea that people experience in the long term. See, constipation occurs because your bowel movements slow down.
But more seriously, GLP-1 therapy is sometimes thought to cause digestion to slow down, leading to gastroparesis. Although gastroparesis is more commonly known as gastric paralysis, the term covers any degree of slowed gastric emptying that is harmful to us. Another serious adverse reaction associated with GLP-1RA use is intestinal obstruction, or intestinal blockage. Last year, the FDA mandated a label change for Ozempic that mentioned the potential risk of intestinal obstruction after an adverse event notification, but did not confirm that intestinal obstruction was a side effect.
Thankfully, intestinal obstruction and gastroparesis appear to be rare complications of GLP-1RA. So far, there hasn’t been strong evidence of some of the other potentially serious side effects, such as an increased risk of suicide or severe muscle loss, although it’s certainly possible that scientists may uncover new health risks that haven’t been identified yet. For now, GLP-1RAs do appear to be safe and effective for most patients who take them, and even the more unpleasant gastrointestinal side effects they cause diminish over time.
The future of obesity
While semaglutide and its brand have become the poster child for a new era of obesity treatment, this is really just the beginning. For example, Eli Lilly’s recently launched tirzepatide, which mimics GLP-1 and another hunger-related hormone, GIP, has been shown to be more effective than semaglutide. Novo Nordisk and other drug companies are also developing their own successors, some of which combine GLP-1 with two other hunger-related hormones. Other companies are working to make these drugs easier to take, and one company is even looking into whether it might be possible to make our cells naturally produce more GLP-1 through a single, lifelong dose of gene therapy.
While all this research may be revolutionary, doctors like Covello point out that these drugs don’t address the root causes of why obesity becomes a bigger problem over time. The adult obesity rate in the United States is currently about 42%, and even since Wegovy was approved in 2021, the prevalence of obesity has continued to rise in many states. A bigger approach to solving this growing public health problem.
“I think we’re going to see more elegant approaches in the future than what we’re seeing now, and hopefully better tolerance. But I think a big question that remains is why are we seeing this widespread Obesity epidemic? Although we have indeed made significant progress in understanding the new mechanisms behind excessive weight gain, this question remains unanswered,” she said. “If we can figure out what’s going on or what’s changed and fix that, then maybe the answer is to fix that problem and not necessarily look to better and better drugs that actually just mimic or enhance what’s natural in the body. signals, and these signals are always designed to deal with metabolism.
Semaglutide and other GLP-1RAs have proven to be more useful than we hoped, and the future for these drugs is bright. But there are some health problems that no drug can solve alone, no matter how miraculous it may seem.